- high on health
- Posts
- high on health (49/2023) - Record Snow, End-of-year Parties, Long COVID, Fluctuating Blood Pressure, HOKA running shoes
high on health (49/2023) - Record Snow, End-of-year Parties, Long COVID, Fluctuating Blood Pressure, HOKA running shoes
Cheers!
This is high on health! Your weekly dose of fresh perspectives, slicing through the noise to bring you the latest in snowfall and COVID.
Many people who tried to travel in, to and from Germany this week faced difficulties due to heavy snowfall that occurred over the weekend. Munich experienced a new snowfall record in December within a day, with 44 cm (17.3 in) of snow. This led to flight and train cancellations, delays, and other disruptions that caused frequent changes to people's schedules. Additionally, the Gewerkschaft Deutscher Lokomotivführer (GDL), the Union of German Train Drivers, called for a strike during the second half of the week. While it's important to fight for fair pay and better work hours, the timing of this strike was not ideal... but may have helped to make the point 😏 👉 ✍️

I still made it to London to meet with colleagues and attend various social gatherings. It’s a year-end season, which is busy with team meetings and dinners to celebrate team members’ accomplishments. This is my favorite part of the year! I'm still recovering from our end-of-year party and can truly say that events like these give me goosebumps - I love our diverse team, the creativity, and the entrepreneurial drive, and I feel privileged to be part of such an inspiring team! 🔥❤️🙌🤝🙏💪
This week my team “family” (= my wife and kids) has been experiencing seasonal sicknesses that are common during this time of year, especially with kids. We are working through it and doing our best to recover before the holidays. I’m cheering on my immune system to stay focused in the last quarter and not catch a buzzer-beater1 of sickness before the holidays. The above-mentioned social gatherings don’t make this an easy win. 👥🎉
The pandemic has changed how we approach the common cold and cough symptoms. Whenever we experience these symptoms, we reach for a COVID test kit.
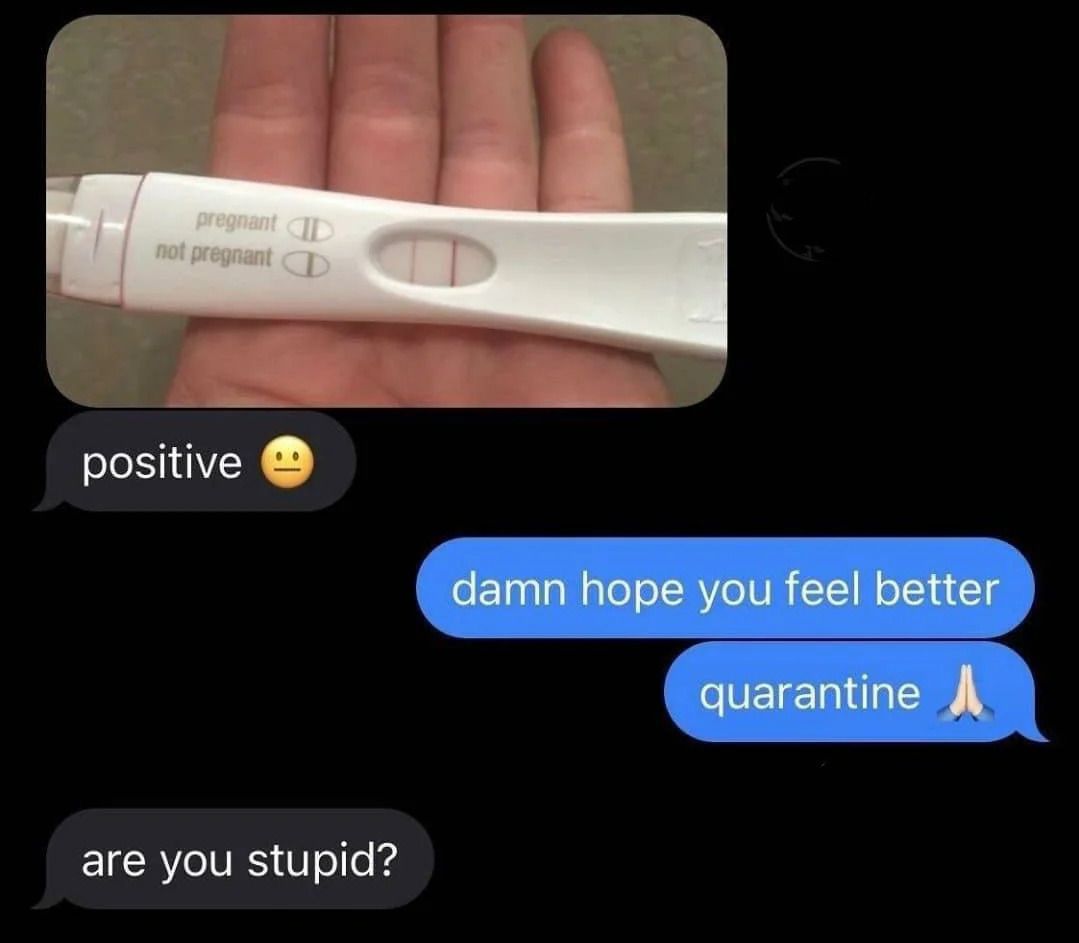
There has been a rise in cases around us recently, with friends and colleagues reporting positive test results. It's hard to say how common COVID is since the numbers are no longer tracked, but it's still affecting many people. I came across a few articles and research updates on the long-term effects of COVID, which are worth sharing. These articles touched on Long COVID or post-COVID conditions, which many people still experience even if they have recovered from the initial symptoms.
Stay safe and healthy out there, and all the best for the final two weeks before the holiday break!
Take care!

PS: Yes, the washing machine is still broken. We have a scheduled appointment for repair on the 11th . Please include us in your prayers.
1 In a defining moment in NBA history, Michael Jordan hit a buzzer-beater against the Cleveland Cavaliers in 1989. With only three seconds left, MJ outsmarted Craig Ehlo and evaded Larry Nance to make the game-winning shot, leading the Bulls to a 101-100 triumph. The iconic image of Jordan's victory fist-pump in the air over a crestfallen Ehlo marked one of the greatest finishes in basketball history.
Stuff I’m reading
Introduction to Long COVID
Welcome to the mysterious world of Long COVID, a post-COVID condition that is both difficult to understand and widespread. While some individuals recover from COVID-19 within a few days or weeks, others experience a prolonged struggle with various symptoms that persist long after the initial recovery. 🕒🤒🦠
Defining the Undefined
The CDC has coined the term "Long COVID" to describe a spectrum of conditions that result from SARS-CoV-2 infection. Known scientifically as post-acute sequelae of SARS-CoV-2 infection (PASC), it has garnered attention from organizations such as the NIH and AMA. The AMA's effort to establish a separate ICD-10 code for Long COVID highlights the medical community's recognition of this condition as more than just a footnote in the pandemic's history. Long COVID is defined as ongoing, relapsing, or new symptoms or conditions present 30 or more days after infection, and symptoms can vary widely in severity and duration. 😣 😣
Long COVID Trends: A Shifting of the Tide?
The CDC uses multiple methods to estimate the number of people experiencing Long COVID. Each approach provides a piece of the puzzle to understand better those experiencing Long COVID. Some studies rely on self-reported symptoms, while others collect symptoms and conditions in medical records. Some studies focus only on people who have been hospitalized, while others include people who were not hospitalized. The estimates for how many people experience Long COVID can vary depending on who is included in the study and how and when the study collected information.
Long COVID shows a higher prevalence in women and predominantly impacts those aged 35 to 49, with a notable trend in rural areas over metropolitan ones. Those with a history of severe COVID-19, requiring hospitalization or intensive care, face a greater risk. Additionally, individuals with pre-existing health conditions and the unvaccinated are more susceptible to developing Long COVID.
Recent US data shows a promising decline in Long COVID’s incidence. This decrease can be attributed to increased immunity, milder virus variants, and new treatments, which bring cautious optimism. Studies, including one by Imperial College London, highlight a lower Long COVID risk with the Omicron variant. The CDC reports a drop from 18.9% in mid-2022 to 11% in early 2023, as echoed by European research.

Symptom Spectrum
Long COVID is a complex condition that can develop after a COVID-19 infection. The symptoms of Long COVID can vary in duration and intensity, lasting from weeks to years after the initial infection. Symptoms can also disappear and reappear unpredictably, making the condition more complicated. 😷🔄⏳
Common Long COVID Symptoms Overview
Each person's experience with Long COVID is unique and characterized by diverse symptoms that can change over time.
General Symptoms: Primary complaints include fatigue significantly impacting daily activities and worsening symptoms after physical or mental tasks.
Respiratory and Heart Symptoms: These encompass breathing difficulties, persistent cough, chest pain, and heart palpitations.
Neurological Symptoms: Cognitive challenges like "brain fog", headaches, sleep disturbances, dizziness upon standing, sensory changes (pins-and-needles), and alterations in smell or taste are common. Mental health issues such as depression and anxiety are also reported.
Digestive Symptoms: These include diarrhea and stomach pain.
Other Symptoms: People with Long COVID often experience joint or muscle pain, skin rashes, and changes in menstrual cycles.
Categorizing the Chaos of Long COVID
The complex puzzle of Long COVID can be categorized into three broad categories based on the symptoms and their impacts.
The first category is the "Ongoing Viral Impact," which includes individuals who experience continuous symptoms due to the initial damage caused by the virus. These lingering effects are the viral echoes that refuse to fade and can impact bodily functions and overall health. 🦠🌊
The second category is "Post-Hospitalization Syndrome," where symptoms stem from extended hospital stays, including time in ICUs or prolonged bed rest. This group may experience issues such as muscle weakness, cognitive changes, and psychological impacts due to the intense medical interventions they underwent. 🏥💪
The third category is "Delayed Symptom Onset," which involves symptoms that surface after apparent recovery. It's like a second wave of health challenges that emerge, adding an unexpected twist to the recovery narrative. These could range from new respiratory issues to neurological symptoms, painting a complex picture of recovery and relapse. 🧠🌪️
Understanding these categories can give us a clearer picture of Long COVID's multi-faceted nature – a condition that defies straightforward explanations and demands a nuanced approach to treatment and care.
Vaccines: A Shield Against Long COVID
Recent research published in the BMJ has revealed that getting vaccinated before the first COVID-19 infection significantly reduces the risk of developing Long COVID. The study, which involved over half a million Swedish adults, found that individuals vaccinated are almost four times less likely to suffer from Long COVID than those who have not been vaccinated. The vaccine's protective effect increases with each dose: a single dose reduces Long COVID risk by 21%, two by 59%, and three or more doses by a remarkable 73%.
This study took place from December 2020 to February 2022 and compared vaccinated individuals (who had received at least one COVID-19 vaccine dose before infection) with unvaccinated individuals. The study tracked the emergence of Long COVID symptoms such as brain fog and fatigue. However, it is important to note that the study focused on the original vaccine formulations and did not consider Long COVID following reinfections. As the pandemic continues to evolve, there are still unanswered questions about how these findings apply in the context of updated vaccinations and multiple infections.

A vial of the COVID-19 vaccine targeting XBB.1.5, made by Pfizer and BioNTech. The study looked only at original COVID-19 vaccines, not newer boosters like this one released this fall.
Antidepressants and Long COVID: A New Treatment Avenue?
Researchers from the University of Pennsylvania have discovered a crucial connection between Long COVID and serotonin levels, which could lead to a new treatment approach. They found that Long COVID patients had lower serotonin levels, a key neurotransmitter affecting various bodily functions such as mood, digestion, and sleep. This discovery, published in the journal Cell, suggests that selective serotonin reuptake inhibitors (SSRIs), commonly used as antidepressants, may be an effective treatment for Long COVID.
The study explains that reduced serotonin levels in Long COVID patients are caused by persistent low-level SARS-CoV-2 infection, inflammation, and overactive blood platelets1 . These factors may explain the wide range of symptoms experienced by Long COVID patients. However, while this research offers new therapeutic possibilities, it is important to proceed cautiously. Further investigation is needed to determine the effectiveness of SSRIs in raising systemic serotonin levels and relieving Long COVID symptoms. Nevertheless, this new understanding of Long COVID's underlying mechanisms provides hope.
Gut Health: A New Ally Against Long COVID?
Researchers at the Chinese University of Hong Kong conducted a trial investigating the potential benefits of altering the gut microbiome in relieving long COVID symptoms. The trial tested a synbiotic formula, SIM01, which combined prebiotics and probiotics, on 463 patients suffering from long COVID symptoms. The results of the study, presented at Digestive Disease Week 2023, showed that patients who received SIM01 experienced significant relief in symptoms related to digestion, fatigue, concentration, memory, and overall malaise.

This synbiotic approach has previously been shown to improve health outcomes in COVID-19 patients and positively impact the gut's microbial composition. This led to an alleviation of various gastrointestinal symptoms and an improvement in overall well-being. While these findings are promising, they require further clarification and validation. Experts highlight the need for additional rigorous research to confirm the effectiveness of SIM01 in treating long COVID comprehensively. Nevertheless, this study is a promising step towards understanding and potentially managing long COVID by modulating gut health.
Symptomatic Relief Strategies
Long COVID results in a variety of symptoms that require personalized treatment. For example, low-dose naltrexone can treat pain and neurological symptoms, while Coenzyme Q10 and D-ribose supplements may help alleviate fatigue. These treatments depend on the patient's needs and align with hospital and national health guidelines. This approach ensures that each patient receives care tailored to their specific symptoms, providing relief and aiding in their recovery.
Embracing Supportive Care
Neurological symptoms such as headaches, cognitive impairment or "brain fog", memory issues, depression, anxiety, and insomnia are common among Long COVID patients. These symptoms require a supportive approach, including cognitive behavioral therapy and counseling. It is essential for primary care physicians to monitor these symptoms and provide reassurance to their patients, as this is vital for their well-being. If necessary, referrals to psychiatric or psychological services should be made, highlighting the importance of a comprehensive and empathetic care strategy.
Rehabilitative Treatment & Self-Monitoring
The recovery from Long COVID is a joint responsibility of healthcare providers and patients. Self-monitoring is crucial, especially for symptoms like post-COVID breathlessness. Patients should track their progress through home-based methods such as daily pulse oximetry readings. This not only aids in recovery by providing tangible proof of improvement but also reassures the patient. Pulmonary rehabilitation, including various breathing exercises, ranging from simple deep breathing to specialized yoga techniques, aims to recondition the diaphragm for improved respiratory function. This combination of self-monitoring and rehabilitative treatment fosters an environment of active patient participation in their recovery journey.
Each aspect of Long COVID care, from symptomatic relief and supportive care to rehabilitation and self-monitoring, is essential to comprehensively managing this complex condition. Adapting these strategies to individual patient needs ensures a holistic approach to treatment and recovery.

Charting New Paths: Understanding and Overcoming Long COVID
Navigating Long COVID is a complex and challenging task that involves dealing with diverse symptoms and evolving research. The effectiveness of vaccines and emerging treatments can change frequently, emphasizing the need for professional and informed approaches when managing this condition. It is important to stay up-to-date with the latest research, employ comprehensive care strategies, and build a knowledgeable community. Keeping up with the latest developments and advocating for advancements in care is crucial.
I hope none of you, your family, or your friends have been affected. But in case someone you know has been affected, I hope they received a comprehensive approach to tackling the issue. I am interested in your stories, and I hope this summary has provided you with some inspiration and updates on the topic.
I would love to get your thoughts and comments!
1 Platelets, or thrombocytes, are tiny and colorless cell fragments in our bloodstream. Their primary function is to form clots and stop or prevent bleeding. Our bone marrow, the spongy tissue inside our bones, produces platelets. Stem cells in the bone marrow develop into red blood cells, white blood cells, and platelets.
Words I’m pondering
When something is important enough, you do it even if the odds are not in your favor.
Science I’m believing
High blood pressure is not the only factor that affects cognitive health. Variability in blood pressure is also important. A study conducted on 70 older adults without dementia showed that those with higher fluctuations in their blood pressure, especially in the short-term and mid-term, had poorer cognitive performance in areas such as attention, psychomotor speed, and executive function. These variations in blood pressure, which various factors can influence, come in different types - from moment-to-moment changes to shifts over several years.
Interestingly, higher short-term systolic blood pressure variability was linked to increased arterial stiffness, a key risk factor for cognitive impairment. This research highlights that blood pressure variability is vital for brain health, not just the average blood pressure level. This indicates that maintaining a stable blood pressure could be important in preventing cognitive decline. 🧠💡
Things I’m graving

Hoka Clifton 9
Just to be transparent, I currently own multiple pairs of different Hoka models because I love them all. I weigh 100kg, used to be a wrestler and now I'm a hybrid athlete who recently decided to train for a marathon due to an early onset midlife crisis. To provide comfort to my knees, I need cushioned running shoes, and Hoka's lineup is just fantastic.
Although some companies have moved on from ethylene vinyl acetate (EVA) foam to newer formulations, Hoka has stuck with its proprietary EVA foam padding and uses various blends of compression-molded EVA (CMEVA) foam, with small variations to fine-tune the shoes for either low weight or strong energy return. CMEVA is found on shoes all across the lineup, including flagship models like the Bondi and Clifton, creating the traditional cushioned feel that Hoka fans like me love. At present, I run a lot in Bondi 8s and even use Clifton’s lifestyle models as my go-to sneakers daily.
The Bondi is a highly cushioned road shoe with a very thick midsole. The latest version of the Bondi keeps the same formula that has earned this shoe a dedicated following: maximum cushioning for a very comfortable ride. The midsole foam is now lighter and even softer than the previous model. For a faster ride, the Bondi X is a good option, as it provides a similar cushioned feel but with an embedded carbon fiber plate for a more responsive and speedy ride.
Love them!

DISCLAIMER: None of this (such as text, graphics, images, and other materials) is medical or health advice. This newsletter is strictly for informational, educational, and entertaining purposes only. While I’m a medical doctor and a dentist by training, I’m not your doctor. The content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on high on health! Please be careful and do your own research.



Reply